

OCD is characterized by recurrent, unwanted, intrusive obsessive thoughts, images or impulses that cause anxiety and by accompanying, compulsive behaviors aimed toward stopping the distress. Obsessions are often distressing or embarrassing and do not make sense. Sufferers often recognize that these thoughts are inconsistent with one's normal self. Compulsions are physical or mental acts used to decrease anxiety and distress elicited by obsessions. OCD is defined by the cause-and-effect relationship between obsessions and compulsions. An estimated that up to one in fifty suffers from OCD at a given time.
OCD can manifest in many ways. Common obsessions include fear of contamination, fear of causing harm, preoccupation with certain numbers, a need for exactness or symmetry, intrusive sexual worries, and excessive perfectionism. Common rituals include checking, compulsive hand washing, ordering and arranging, repeating special numbers or prayers, rewriting or rereading work or school assignments, mental reviewing and reassurance seeking. A comprehensive list of obsessions and compulsions can be found on the Yale-Brown Obsessive Compulsive Scale. People with OCD commonly avoid situations that make them anxious.
Since engaging in rituals can be exhausting, OCD sufferers often avoid situations that may elicit their fears. While engaging in compulsive behaviors alleviates anxiety in the short run, in the long term, rituals function to maintain obsessions.
The best known treatment for OCD is Exposure and Response Prevention (ERP), a form of Cognitive Behavioral Therapy that teaches OCD sufferers to face feared situations while refraining from engaging in compulsions. With repeated exposure and ritual prevention, OCD sufferers learn that:
ERP can be challenging at first, but most people find that therapy gets easier if they stay with it. Most experience vast improvement in approximately 17 sessions.
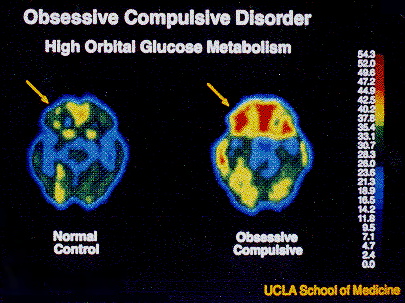 OCD is a genetic brain disease that most likely also has environmental factors. Treatment addresses current symptoms of OCD through exposure and response prevention, rather than trying to understand the source of the problem. PET scan studies showing brain images of OCD sufferers before and after ERP suggest that ERP alters the brain so that individuals with OCD have brains that function more like those without OCD after this treatment.
OCD is a genetic brain disease that most likely also has environmental factors. Treatment addresses current symptoms of OCD through exposure and response prevention, rather than trying to understand the source of the problem. PET scan studies showing brain images of OCD sufferers before and after ERP suggest that ERP alters the brain so that individuals with OCD have brains that function more like those without OCD after this treatment.
For additional information about Exposure and Response Prevention for OCD, please visit the International OCD Foundation website at www.ocfoundation.org.
Photo source: Baxter LR, Schwartz JM, Bergman KS, et al: Caudate glucose metabolic-rate changes with both drug and behavior-therapy for obsessive-compulsive disorder. Arch Gen Psychiatry 1992; 49:681-689.